A Modified Peptide Shows Promise For Fighting Tumors
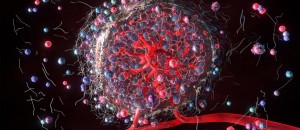 The growth of healthy tissues in the body depends on the development of new blood vessels, a process called angiogenesis, that enable proper blood flow, meaning nutrients and oxygen are delivered while toxic metabolic products are removed. But solid tumors grow faster than healthy tissues, resulting in deficiencies in oxygen and blood flow, which leads to accelerated formation of dysfunctional blood vessels. Malignant cells rapidly grow while antitumor immune cells quickly lose their viability and function.
The growth of healthy tissues in the body depends on the development of new blood vessels, a process called angiogenesis, that enable proper blood flow, meaning nutrients and oxygen are delivered while toxic metabolic products are removed. But solid tumors grow faster than healthy tissues, resulting in deficiencies in oxygen and blood flow, which leads to accelerated formation of dysfunctional blood vessels. Malignant cells rapidly grow while antitumor immune cells quickly lose their viability and function.
These events, cell biologist Serge Fuchs of the School of Veterinary Medicine says, promote generation of the immunosuppressive tumor microenvironment, which stimulates the spread and growth of tumors and confers resistance to antitumor therapies.
Past research has shown how native C-type natriuretic peptide (CNP), a 22-amino acid peptide produced by endothelial cells and fibroblasts, stimulates growth of normal blood vessels and restores proper blood flow and oxygenation within tissues of rodent limbs that weren’t getting enough blood flow. Given the importance of CNP in angiogenesis, researchers reasoned that CNP would also play a critical role in regulating tumor vasculature. But therapeutic potential of CNP is severely hampered by its short half-life of less than three minutes, says Zhen Lu, a former senior research investigator in Fuchs’ lab.
Fuchs and Lu are part of an interdisciplinary, collaborative team which found that modifying CNP stimulated the formation of blood vessels, increased blood flow through tissue, reinvigorated antitumor immune responses, and slowed growth of tumors in an animal model. The results published in the journal Science Translational Medicine suggest that the treatment could alleviate hypoxia, or insufficient oxygen levels, in tumors. The team includes researchers from Kyushu University, the Higashiosaka City Medical Center, the Case Western Reserve University School of Medicine, and PharmaIN Corp.
“It is a successful approach to target the immunosuppressive tumor microenvironment, which should lead to a breakthrough in treatment of a large variety of solid tumors,” says Fuchs, a corresponding author on the paper.
The researchers successfully tested dCNP in several mouse solid tumor models, including pancreatic, colon, lung, and mammary adenocarcinomas, along with hepatocellular carcinoma and osteosarcoma.
Fuchs says PharmaIN generated the dCNP treatment, researchers from Kyushu University and the Higashiosaka City Medical Center in Japan identified its antitumor effects, and scientists from Penn Vet, the Perelman School of Medicine, and the School of Arts & Sciences examined the mechanism of action.
Fuchs explains that this research builds on the work of Judah Folkman and Rakesh Jain that looked at vascular endothelial growth factor (VEGF), a signaling protein that accelerates the formation of dilapidated and leaky blood vessels. They proposed anti-VEGF therapy. But resistance to anti-VEGF agents and difficulties with precise dosing meant obstacles remained to solving the problem of the immunosuppressive tumor microenvironment.
Lu says the new study demonstrates that, instead of inhibiting dysfunctional tumor angiogenesis by anti-VEGF agents, inducing healthy vasculature by dCNP could reinvigorate anti-tumor immunity and improve solid tumor therapies. “This study proposed a new paradigm for anti-angiogenic therapy and provided opportunity for developing new anti-angiogenic medication in the future,” he says.
Fuchs says researchers completed preclinical studies and PharmaIN completed toxicity profiles, so the next step is selecting a solid tumor model for clinical trials.
Serge Y. Fuchs is the Elizabeth and William Whitney Clark Professor of Oncology, professor of cell biology in the Department of Biomedical Sciences, and director of the Mari Lowe Center for Comparative Oncology at the University of Pennsylvania School of Veterinary Medicine.
Zhen Lu is a professor of oncology and pharmacology at the Institute of Drug Discovery and Development at China Pharmaceutical University and a former senior research investigator in Fuchs’ lab at Penn Vet.
The other co-authors are Daniel P. Beiting, Ellen Puré, Rong Qiu, Zebin Xiao, and Menghao You of Penn Vet; Sandra Bicher, Yi Fan, Terence P. Gade, Subin S. George, Constantinos Koumenis, George McClung, Ben Z. Stanger, and Ioannis Verginadis of the Perelman School of Medicine; Zhen Miao and Wei Guo of the Department of Biology in the School of Arts & Sciences at Penn; Yoshinori Fujimura, Yui Hatakeyama, Motofumi Kumazoe, Hiroaki Onda, Hirofumi Tachibana, and Yasutake Tanaka of Kyushu University; Elijah M. Bolotin, Nikolay M. Buynov, Katrina Bykova, Gerardo M. Castillo, Rebecca E. Guerra, Akiko Nishimoto-Ashfield, and Yao Yao of PharmaIN Corp.; Takashi Nojiri of the Higashiosaka City Medical Center; and J. Alan Diehl of the Case Western Reserve University School of Medicine.
This research was supported by the National Cancer Institute at the National Institutes of Health (grants R01 CA247803, R01 CA240814, and P01 CA165997); National Heart, Lung, and Blood Institute at the National Institutes of Health (grants R44HL134448 and R44HL156295); and a Sponsored Research Agreement with PharmaIN Corp.
Short URL: https://caninechronicle.com/?p=301151
Comments are closed